A primary care focus: Nondental providers use fluoride varnish as part of well-child checkups
By Christine Nathe, RDH, MS
The idea of incorporating primary dental care into settings other than the dental office is nothing new. Just take a look back 100 years or so, when Dr. Alfred Fones envisioned dental care in school systems. The latest trend, which is still growing, is the incorporation of primary dental care, specifically the application of fluoride varnish, during routine well-child checkups at the doctor's office. While this is not without controversy, it does have the promise of increasing access to care for some children who might otherwise live without the benefit of topical fluoride application.
Scope of practice
Opposition to this new trend comes from those concerned about practice loss for dental providers. However, this could potentially increase the scope of career opportunities for dental hygienists, which would include the training of nondental providers in the application of topical fluoride and other primary dental concepts. In fact, dental hygienists could coordinate the training and use of this preventive strategy throughout primary care systems, pediatric clinics, and doctors' offices.
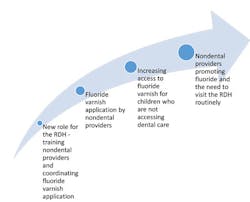
Moreover, this could provide a large voice for dentistry as a whole. Educating medical and nursing providers on preventive dentistry, including fluoride varnish application, could lead to promoting dental health concepts that have not been realized on such a grand scale before. Imagine physicians routinely discussing fluoride with patients, as well as the need to visit the dentist and dental hygienist on a regular basis. This could result in an increased use of dental services by many people (see Figure 1).
There are many reasons children may not be accessing dental care. These include issues such as appointment availability, transportation difficulties, lack of financial resources, lack of understanding about dental health status, and much more. The overriding barrier is that many parents do not value the provision of dental prevention and therefore wait until the child needs restorative dental care, or worse, until the child requires anesthesia for treatment of severe disease or infection.
Figure 1: Primary dental care integration
Figure 2: Steps in accessing dental care
It's difficult to argue that the integration of preventive dental services within primary care or pediatric clinics would undoubtedly increase access to dental prevention for children, or that this access could lead to the adoption of values necessary to routinely access dental care. This could be very important since most reports suggest that less than half of Americans routinely access dental care (see Figure 2).
Fluoride varnish
Topically applied fluoride varnishes have been used extensively as a professional preventive strategy for years,1 although the use of fluoride varnish for caries prevention is technically considered an "off-label" use.2 How often to apply fluoride varnish varies depending on the risk to the patient, particularly for children with higher risk.3
The Cochrane Review, which analyzed research on children and adolescents with permanent teeth, found that young people treated with fluoride varnish experienced on average a 43% reduction in decayed, missing, and filled tooth surfaces. This included reviewing 13 trials. In the 10 trials that specifically assessed the effect of fluoride varnish on deciduous teeth, evidence suggests a 37% reduction in decayed, missing, and filled tooth surfaces. Additionally, there was little information concerning possible adverse effects or acceptability of treatment.4
More pediatricians are reportedly integrating the use of fluoride varnish and other preventive dental services, such as caries risk assessments and oral exams, into their practices. But this is still a very new and uncommon addition. Roberts and Erwin conducted a study on the use of fluoride varnish in pediatrician offices in Tennessee and found that although the majority reported that they are likely to examine children's teeth during well-child-care visits, only a few use preventive techniques such as application of fluoride varnish. They stated that they received very little education on oral health during medical school and residency programs.5
Tellez and Wolff stated that fluoride varnish treatments are attractive because they can be easily incorporated into well-child visits and community-based geriatric programs.6 Rolnick et al. reported that fluoride varnish programs can be introduced and sustained in the primary care setting.7 Lewis, Lynch, and Richardson stated that fluoride varnish could be adopted successfully into medical practices with physician and staff commitment, motivational training, appropriate systems, and resources for professional dental care referral.8 More studies need to be conducted on this integration, and dental hygienists have a prime opportunity to facilitate and lead this research.
Billing by nondental providers
Dental hygienists are familiar with CDT (Code on Dental Procedures and Nomenclature) codes, the mechanism for billing dental services. CDT codes are developed and maintained by the American Dental Association. Medical and nursing providers use the CPT (Current Procedural Terminology) codes that are developed and maintained by the American Medical Association.
In January 2015, a new CPT code for medical and nursing providers was created. This code, labeled Code 99188, application of topical fluoride varnish by a physician or other qualified health-care professional, is for the application of fluoride varnish by medical or nursing providers.9 Interestingly, the US Preventive Services Task Force (USPSTF) recommended this for children up to 6 years of age; therefore, code 99188 must be covered by commercial insurance for children up to age 6. This increases the likelihood that these children will benefit from the application of fluoride varnish.
Current American Association of Pediatric Dentistry (AAPD) policy supports fluoride application by auxiliary dental personnel or other trained allied health professionals, by prescription or order of a qualified dentist, and after a comprehensive oral examination has been performed.10 Moreover, the ADA has a long history of promoting child well-being and medical-dental partnerships. In 2004, the ADA House of Delegates passed a policy stating that physicians and their properly trained and supervised designees be allowed to provide preventive dental services to infants and young children.11 Dental hygiene was created to provide care within health and educational systems as collaborative providers. A review of current ADHA policies reveals that this initial collaborative vision has become even stronger.12
The American Academy of Pediatrics (AAP) has an entire page on its website that explains the tools necessary for fluoride varnish and other preventive dental strategies into practices.13
Additionally, the American Public Health Association (APHA) has written policy regarding the application by various providers with public health, dental, and medical practice.14
Nondental providers can fill the void for many children in need of preventive treatment. Evidence suggests that fluoride varnish significantly decreases dental caries in children. Multiple associations support the incorporation of basic preventive dental services by nondental providers, and the AMA recently created a code for nondental providers to bill for the application of fluoride varnish on children. Dental hygienists can help prevent dental decay in vulnerable patients by teaming up with physicians and nurses to train and coordinate basic preventive dental services in health systems. This also increases career opportunities for dental hygienists.! RDH
CHRISTINE NATHE, RDH, MS, is director at the University of New Mexico, Division of Dental Hygiene, in Albuquerque, N.M. She is also the author of "Dental Public Health Research" (www.pearsonhighered.com/educator), which is in its third edition with Pearson. She can be reached at [email protected] or (505) 272-8147.
References
1. Azarpazhooh A, Main PA. Fluoride varnish in the prevention of dental caries in children and adolescents: A systematic review. J of Can Dent Assoc, (2008) 74:73-79. Retrieved from https://www.cda-adc.ca/jcda/vol-74/issue-1/73.pdf. 2. Beltran-Aguilar ED, Goldstein JW, Lockwood SA. (2000). Fluoride varnishes-A review of their clinical use, cariostatic mechanism, efficacy and safety.10. Talking Points AAPD Perspective on Physicians or Other Non-dental Providers Applying Fluoride Varnish. June 2006 Edition. Retrieved from http://www.mychildrensteeth.org/assets/2/7/1225.pdf.
11. Manchir M. Pediatricians seek collaboration with dentists on fluoride varnish. ADA News. August 7, 2015. Retrieved from http://www.ada.org/en/publications/ada-news/2015-archive/august/pediatricians-seek-collaboration-after-new-task-force-recommendation-on-fluoride-varnish?nav=news.
12. ADHA Policy Manual: Public Health. Retrieved from https://www.adha.org/resources-docs/7614_Policy_Manual.pdf.
13. American Association of Pediatrics. Children's Oral Health. Retrieved from http://www2.aap.org/oralhealth/PracticeTools.html.
14. American Public Health Association. Fluoride Varnish for Caries Prevention Policy. Retrieved from https://www.apha.org/policies-and-advocacy/public-health-policy-statements/policy-database/2014/07/09/07/51/fluoride-varnish-for-caries-prevention.
Additional Resources
ADA Center for Evidence-Based Dentistry. Topical Fluoride for Caries Prevention. (2013) Retrieved from: http://ebd.ada.org/~/media/EBD/Files/Topical_fluoride_for_caries_prevention_2013_update.ashx